DEMO DEVICES: Transforming the Patient Experience With Demonstration and Training Devices
A patient named “Ruth” is sitting in her doctor’s office, waiting to hear about the outcome of her recent physical exam, lab work, and imaging studies. Her doctor enters and informs her of her diagnosis and starts to review her prospective care plan, the procedures she will need to undergo, the medications she will need to take, and the device she will need to use to administer one of the medications. In addition, her doctor tells her that before she can administer that medication, it must be reconstituted.
As her doctor speaks, Ruth tightens her grip on the armrests of the chair, and her heartrate quickens. An overwhelming mix of feelings creeps into her, narrowing her scope of comprehension. She wishes she had a notepad, or better yet, a family member or friend who was there with her and could take notes for her—and hold her hand, while they were at it. Her mind floods with questions, but she isn’t able to center on any one question long enough to fully form and articulate it. As Ruth struggles to process all of this information, she vaguely hears her doctor’s voice saying, “And, don’t miss a dose. Also, remember that this medication must be refrigerated.” At this moment, Ruth isn’t sure she would remember that or much of anything right now. In fact, all she really knew was that the symptoms she had been experiencing for the last few months meant she had a disease, a disease with a name that she never had heard of before.
Medical Devices Are Integral to Disease Management
As the patient scenario above illustrates, the diagnosis of a disease or condition can be a difficult and overwhelming experience. Yet, we rely on modern medicine, including advanced medical devices, to treat and manage disease and improve the quality of life of patients.
Medical devices are used in many settings, including the self-administration of medication at home without medical supervision or training. Some examples of medical devices that enable patients to self-administer medication at home include the following [1]:
According to the World Health Organization, there are an estimated 2 million types of medical devices on the global market [2].
Autoinjectors, including pens or on-body injectors
Prefilled syringes
Nebulizers
Inhalers
Pumps
Nasal sprays
Transdermal systems
of older adults have at least
one chronic health condition
of older adults have at least
two chronic health conditions
Changes in healthcare, patient needs, and technology
A combination of other factors reflecting current changes in healthcare, patient needs, and technology are driving the increased need for medical devices for self-administration.
Healthcare
Staff shortages
Financial pressures
Need to foster improved patient compliance/outcomes
Patient needs
Interest in and convenience of self-administration
Increased requirements for frequent or routine treatments
Patient empowerment and desire to play a greater role in personal care plan
Increased interest in treatment ownership and less reliance on healthcare providers
Reduction in need for transportation, time, and out-of-pocket costs
Need for immediate treatment during emergency situations
Technology
Increase in innovative and patient-friendly device designs
Reformulation of first-generation biologics
Increase in biopharmaceutical approvals [7], [8]
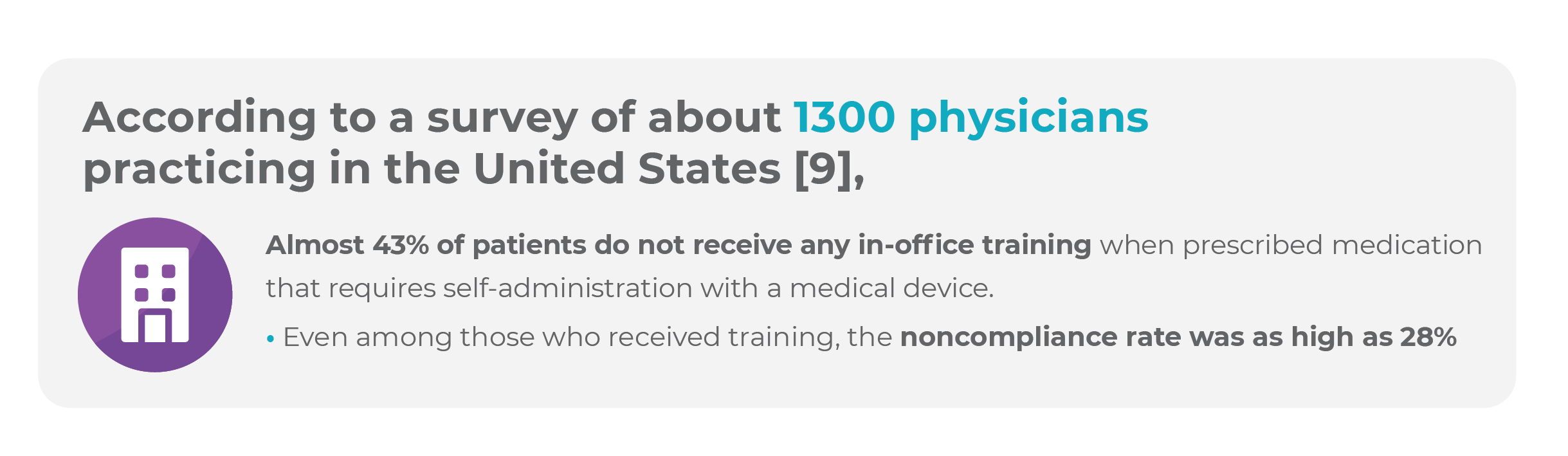
Dismaying Statistics Point to a Need for Improved Medical Device Training
User errors are common: Approximately 50% of patients do not take medications as prescribed, especially those living with chronic conditions [11].
The impact of patient errors varies widely. For example, patients self-administering asthma medication may decrease, but not eliminate, the dose delivered. However, misuse of an epinephrine injector may result in death [10].
User errors in medication self-administration contribute to several adverse outcomes in patient care:
Poor treatment adherence
Increased hospitalizations
Higher healthcare costs
Impact of poor adherence
Every year in the United States, poor adherence is estimated to cause 125,000 deaths, or 10% of hospitalizations, and as much as $300 billion dollars in avoidable healthcare costs [12].
Poor adherence may also contribute to medication waste, disease complications and progression, reduced functional abilities, lower quality of life, and increased mortality [13], [14].
The Forgetting Curve
Another factor that may contribute to poor adherence is the “forgetting curve” theory, postulated by Herman Ebbinghaus, the first psychologist to study memory and learning. This theory suggests that the retention of information worsens over time without practice and recall [15].
According to this theory [16],
50% of the information received from healthcare professionals is forgotten within 1 hour
80% is forgotten within 2 days
90% is forgotten within 1 week
Exacerbating this problem is the occurrence of a stressful event, such as a diagnosis of a disease or chronic condition, which can negatively impact the ability to form and store information. In addition, complex material such as medical information or instructions may be harder to remember [15].
Bridging the Gap With Transformative Patient Education and Training
Treatment success is largely associated with adherence to therapy. Following the prescribed medication dosing regimen consistently is essential for safety, efficacy, and improved patient outcomes.
Ensuring that patients self-administer medications correctly is a critical step toward proper adherence to therapy. For a medication to be effective, it must be delivered to the intended target site to treat the disease, condition, or symptom effectively. Although this task is itself complex, requiring self-administration with a medical device can compound this challenge [11].
Proper self-administration techniques require effective training and education
The challenges of adherence can also be increased by the risk of serious side effects associated with many medications and by the burden of having to take multiple drugs. Such dangers become apparent particularly when a patient takes too much or too little of a medication or else misses a dose or takes an extra one.
Most patients can learn to self-administer their medication safely and effectively if they are properly educated, trained, and supported [18].
Medical device manufacturers often provide instructions for use (IFU) or a demonstration video or instructions on their website. Unfortunately, the IFUs may be difficult for patients to understand, and the use of online resources requires patients to have knowledge of and access to the Internet. The task of navigating, downloading, and reviewing and understanding the appropriate resources can be burdensome and overwhelming for both patients and their caregivers [9].
Patient education and demonstration and training devices
By providing patient education and training, you are telling a patient, “You’re not alone.”
When patients are given the right information at the right time, they are set up for success. In this case, success means patients are more compliant with their therapy, have a better chance of receiving the full benefits of treatment, and may have improved outcomes and quality of life.
In addition, informed patients better understand their treatments and are more likely to be engaged and motivated to be fully involved in their own care.
Demonstration and training devices can be integral to patient education and training
As Ruth’s story demonstrated, undergoing a new therapy that requires self-administration with a medical device may be an intimidating experience for many patients. With demo and training devices, patients can adopt new therapies and medical devices more easily.
Demo and training devices look and function similarly to the actual medical devices they replicate, but they operate without the medication or needles or other sharps required by the actual devices. These tangible and interactive tools allow patients to simulate the treatment administration experience safely and in the convenience and comfort of their own home. A demo device enables patients to handle and interact with the device to become familiar with it and, optimally, be comfortable and efficient with the required preparation steps and user techniques. It also provides an opportunity for patients to cotrain with a caregiver or loved one.
By gaining confidence and empowerment through using a device they understand, patients may be less anxious and more compliant with therapy, and they may commit fewer user errors. For a patient with a serious or chronic condition, proper self-administration technique may become an essential lifesaving skill.
The practical training sessions provided by a demo and training device can improve the patient experience, have positive effects on patient adherence and compliance, optimize treatment and patient outcomes, reduce the training burden on the healthcare staff, and positively impact healthcare providers, pharmaceutical companies, and payers by decreasing healthcare costs.
How Can Artcraft Health Help?
At Artcraft Health, we develop tools, resources, and initiatives that not only educate and train patients, but empower them as well. We can help you to optimize your efforts so both patients and healthcare professionals can build the skills and knowledge needed to ensure better outcomes and the best care possible.
Our experienced team can help you create a wide range of end-to-end solutions, including training kits, step-by-step IFUs, human factors studies, live-action videos, 2D and 3D animations, video brochures, quick reference guides, and other instructional materials.
Through reverse engineering of actual devices, our demo device team can design demonstration and training devices that teach and empower patients to self-administer medication efficiently. In addition, we’ve launched a proprietary technology for device onboarding called accuDemo™, is which is designed to prevent 100% of patient errors in every training session.
AccuDemo is a self-contained device onboarding system in which the original demonstration device is synced via Bluetooth to a digital user interface. This system guides patients step-by-step through device setup and usage, preventing errors in real time by seamlessly withholding access to the next step until the current step is completed correctly. The result is 100% error-free patient onboarding.
About the Author
Linda J. Lamb (Lipp) is a senior medical writer at Artcraft Health.
References
1. Combination product definition combination product types. US Food and Drug Administration website. Updated February 15, 2018. Accessed July 10, 2023. www.fda.gov/combination-products/about-combination-products/combination-product-definition-combination-product-types
2. Medical devices. World Health Organization website. Accessed July 5, 2023. www.who.int/health-topics/medical-devices#tab=tab_1
3. Population Reference Bureau (PRB). Fact sheet: aging in the United States. Published July 15, 2019. Accessed July 6, 2023. https://www.prb.org/aging-unitedstates-fact-sheet/
4. Mather M, Jacobsen LA, Pollard KM. Population Reference Bureau (PRB). Population bulletin: aging in the United States. Vol. 70, No. 2; December 2015. Accessed July 6, 2023. www.prb.org/wp-content/uploads/2019/07/population-bulletin-2015-70-2-aging-us.pdf
5. Caplan Z. 2020 Census: 1 in 6 people in the United States were 65 and over. United States Census Bureau. Published May 25, 2023. Accessed July 10, 2023. www.census.gov/library/stories/2023/05/2020-census-united-states-older-population-grew.html
6. Get the facts on healthy aging. National Council on Aging website. Published March 13, 2023. Accessed July 10, 2023. www.ncoa.org/article/get-the-facts-on-healthy-aging
7. Roy A, Geetha RV, Magesh A, Vijayaraghavan R, Ravichandran V. Autoinjector – a smart device for emergency cum personal therapy. Saudi Pharm J. 2021;29:1205-1215.
8. I’ons G. Self-administration: what drug-delivery device manufacturers should know. Medical Device and Diagnostic Industry website. Published June 11, 2020. Accessed July 18, 2023. www.mddionline.com/drug-delivery/self-administration-what-drug-delivery-device-manufacturers-should-know
9. Lang V, Nalan D. Combination product patient training: how are patients trained and who conducts the training? Presented at: American Society of Mechanical Engineers Medical Devices Conference; April 9-12, 2018; Minneapolis, MN. https://doi.org/10.1115/DMD2018-6956
10. Potera C. Misuse of Autoinjectors and Inhalers. Am J Nurs. 2015;115(3):17. https://journals.lww.com/ajnonline/Pages/ArticleViewer.aspx?year=2015&issue=03000&article=00012&type=Fulltext
11. Zhao M, Hoti K, Wang H, Raghu A, Katabi D. Assessment of medication self-administration using artificial intelligence. Nat Med. 2021;27:727-735. www.nature.com/articles/s41591-021-01273-1
12. Baryakova TH, Pogostin BH, Langer R, McHugh KJ. Overcoming barriers to patient adherence: the case for developing innovative drug delivery systems. Nat Rev Drug Discov. 2023;22(5):387-409. https://pubmed.ncbi.nlm.nih.gov/36973491/
13. McGuinness T, Worley J. Promoting adherence to psychotropic medication for youth-part 1. J Psychosoc Nurs Ment Health Serv. 2010;48(10):19-22. https://pubmed.ncbi.nlm.nih.gov/20873702/
14. Jimmy B, Jose J. Patient medication adherence: measures in daily practice. Oman Med J. 2011;26(3):155-159. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3191684/
15. Ebbinghaus forgetting curve. Practical Psychology website. Published September 15, 2022. Accessed July 24, 2023. https://practicalpie.com/ebbinghaus-forgetting-curve/
16. Kohn A. Brain Science: The forgetting curve – the dirty secret of corporate training. Learning Guild website. Published March 13, 2014. Accessed July 24, 2023. www.learningguild.com/articles/1379/brain-science-the-forgetting-curvethe-dirty-secret-of-corporate-training/
17. Lindenfeld J, Jessup M. “Drugs don’t work in patients who don’t take them” (C. Everett Koop, MD, US Surgeon General, 1985). Eur J Heart Fail. 2017;19(11):1412-1413. https://onlinelibrary.wiley.com/doi/10.1002/ejhf.920
18. Neu K. Helping patients with self-administration of medications. cnaZone website. Accessed July 27, 2023. https://cnazone.com/Helping-Patients-with-Self-Administration-of-Medications-Ceu